|
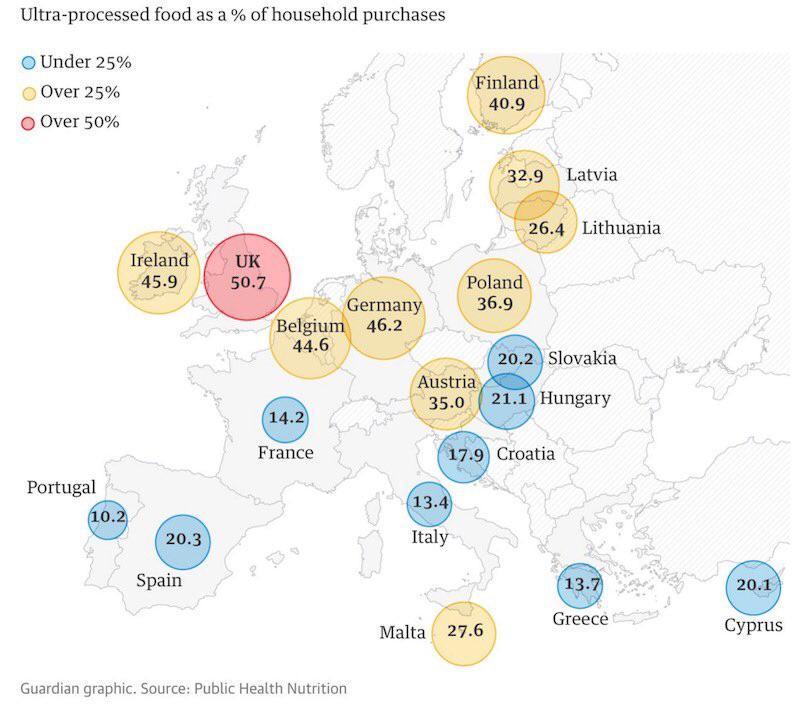
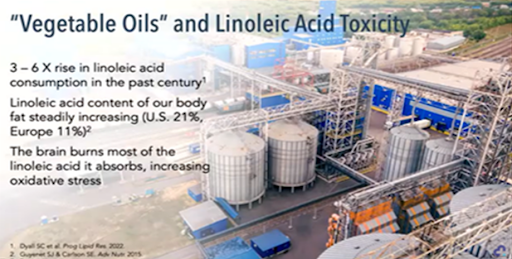
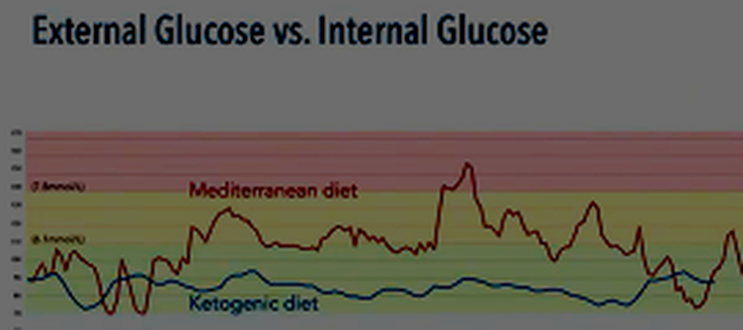
How do our eating habits impact the brain? In terms of eating habits, the UK leads Europe with the highest percentage of food consumed as ultra-processed foods, at 51%. Although still behind America and the Middle East, we are catching up quickly. But why is ultra-processed food a problem? How does it cause oxidative stress and inflammation? Ultra-processed foods contain advanced glycated end products (AGEs) that cause neural inflammation and oxidative stress. These AGEs raise blood and brain sugar levels beyond normal levels, causing excess sugar to stick to proteins, DNA, and lipids in the brain. This caramelisation of important components forms clusters known as AGEs, which are responsible for aging the brain and other tissues in the body. Research has shown their impact on arthritis in the knee and tendon issues in the shoulder. Athletes and active individuals can either accelerate or prevent these issues by improving their diet and overall health. The brain does not passively allow this inflammatory response to interfere with normal cell function. It reacts to the inflammation by raising stress and activating the immune system, using inflammatory cytokines and reactive oxygen species to clear away the problem. This is a normal and healthy response, but it should be targeted, controlled, and temporary. However, if you consume refined carbohydrates or the wrong carbohydrates too often throughout the day, you experience chronic, uncontrolled inflammation and oxidative stress. re to edit. Refined fats have also gained attention recently. Vegetable oils, which have been a major part of our diet since the 1960s, contain linoleic acid (Omega 6 FA). Some argue that it is essential, but linoleic acid is a very fragile Omega 6 FA that easily goes rancid both in your kitchen and in your body. It is highly susceptible to oxidative stress. Over the past 60 years, the levels of linoleic acid in our bodies have increased significantly. While it is present in natural plants and animal foods at low levels, it is now 3-6 times more abundant, as seen in people's body fat. A healthy level would have been around 2%, compared to the levels we see today. Moreover, the brain is not designed to store fat. Instead, it relies on burning glucose and ketones for energy. Burning fatty acids, such as those found in refined fats, leads to more oxidative stress and inflammation, which is the opposite of what should be happening. So, how does oxidation and inflammation affect mental health problems? One way is by throwing neurotransmitters out of balance, including those targeted by psychiatric medications. Excessive oxidative stress and inflammation from the diet can cause this imbalance, along with other environmental factors like smoking and alcohol consumption. While diet is not the sole factor, it is one of the most powerful and easiest to address. As Dr. Georgia Ede says, "The most powerful way you can change your brain chemistry is through food because that's where your brain chemicals come from in the first place." For example, the essential amino acid tryptophan, obtained from dietary protein, can be used to make serotonin and melatonin. However, under the influence of inflammation and stress, less tryptophan goes towards serotonin and melatonin production and more goes towards the glutamate pathway. This leads to an imbalance between glutamate and GABA, the calming and excitatory elements of the brain, respectively. Excessive glutamate can cause damage to proteins, lipids, nucleic acids, mitochondria, and the blood-brain barrier. It can also shrink the hippocampus, which is responsible for learning and memory. Insulin resistance, another factor influenced by diet, also affects the brain. When insulin receptors at the blood-brain barrier become resistant to insulin, the brain experiences a paradox. While glucose levels rise in the blood, brain glucose levels rise also but as insulin rises in the body it becomes unable to get into the brain and this fall due to the lack of insulin metabolism causes and energy crisis for the brain as the glucose cant be used. This leads to cerebral glucose hypometabolism which means its swimming in a pool of glucose unable to be used properly and this condition is strongly associated with Alzheimer's disease and plays a causal role in its development. There is a tight connection between psychiatric conditions such as depression, PTSD, bipolar disorder, schizophrenia, obesity, and insulin resistance. Metabolic psychiatry seeks to understand the relationship between metabolism and brain health. Metabolic health and mental health are intertwined. To support a healthy brain, Dr. Georgia Ede suggests three principles. First, nourish the brain by including adequate amounts of essential nutrients, which must include animal foods. Second, protect the brain by avoiding ingredients that damage it, such as refined carbohydrates and fats. Lastly, energise the brain by providing a reliable energy source that supports healthy brain metabolism over the lifespan, which involves maintaining healthy blood sugar and insulin levels. The evidence shows that the Mediterranean diet, compared to the Standard American Diet, leads to improvements in depression scores. However, the Mediterranean diet still falls short in terms of nourishing, protecting, and energising the brain. It includes nutrient-poor foods like grains and legumes making up the majority of the diet and therefore high in anti nutrients. In terms of protecting the brain, it encourages refined grains known to cause oxidative stress, and also advocates to drink red wine which is a known neurotoxin, a powerful promotor of oxidative stress, and is highly addictive. Finally with respect to energising the brain it is too high in Carbohydrates for people with Insulin Resistance the one thing they need to manage better. The ketogenic diet has been found to have positive effects on various mental health conditions. It was initially developed to stabilise brain chemistry for epilepsy patients and has shown to achieve more than 50% seizure control in randomised controlled trials (RCTs).
Research is currently underway to measure the effects of the ketogenic diet on conditions such as schizophrenia and bipolar disorder through the Metabolic Mind organization. The brain is one organ, and therefore we can suspect that improvements in one area can lead to improvements in all brain-related illnesses. In a study on serious mental illness, participants following the ketogenic diet showed a 20-point improvement in the MADRS scale, indicating a significant improvement in depression scores. All participants in the study showed improvement, which is not typically seen in standard psychiatric care. Additionally, participants experienced significant weight loss despite being on anti-psychotic medications known for weight gain. On average, participants lost 5% of their total body weight, and 63% of them were able to reduce their medication dosage. These findings suggest that the ketogenic diet may have potential benefits for individuals with serious mental illnesses and could be a valuable adjunct to standard psychiatric care. Further research is needed to explore its effectiveness in these conditions. To learn more To find out more about Nutritional and Metabolic Psychiatry please go to https://www.metabolicmind.org/ search for clinicians https://www.diagnosisdiet.com/directory https://www.diagnosisdiet.com/training and Book release January 2024 Change your diet, change your mind, Georgia Ede, MD. Book: Christopher M Palmer, MD ‘Brain Energy’ Rees, J. D., Stride, M., & Scott, A. (2014). Tendons--time to revisit inflammation. British journal of sports medicine, 48(21), 1553–1557. https://doi.org/10.1136/bjsports-2012-091957 Longo, U. G., Franceschi, F., Ruzzini, L., Spiezia, F., Maffulli, N., & Denaro, V. (2009). Higher fasting plasma glucose levels within the normoglycaemic range and rotator cuff tears. British journal of sports medicine, 43(4), 284–287. https://doi.org/10.1136/bjsm.2008.049320 Yang, L., Zhang, J., Ruan, D., Zhao, K., Chen, X., & Shen, W. (2020). Clinical and Structural Outcomes After Rotator Cuff Repair in Patients With Diabetes: A Meta-analysis. Orthopaedic Journal of Sports Medicine. https://doi.org/10.1177/2325967120948499 Fox, A. J., Bedi, A., Deng, X. H., Ying, L., Harris, P. E., Warren, R. F., & Rodeo, S. A. (2011). Diabetes mellitus alters the mechanical properties of the native tendon in an experimental rat model. Journal of orthopaedic research : official publication of the Orthopaedic Research Society, 29(6), 880–885. https://doi.org/10.1002/jor.21327 PMID: 29180223 PMID: 27246996 Tomas Hajek, Cynthia Calkin, Ryan Blagdon, Claire Slaney, and Martin Alda. Type 2 Diabetes Mellitus: A Potentially Modifiable Risk Factor for Neurochemical Brain Changes in Bipolar Disorders Biological Psychiatry February 1, 2015; 77:295–303 PMID: 28097367 Insulin Resistance is Related to Psychiatric Disorders Among Obese Children Özalp Kızılay D et al. 2018. Insulin Resistance is Related to Psychiatric Disorders . https://rdcu.be/dfEYV The Ketogenic Diet for Refractory Mental Illness: A Retrospective Analysis of 31 Inpatients PMID: 30082050 PMID: 7852887
0 Comments
|
Taylormade
|
PERFORMANCE AND REHABILITATION CLINIC
Injury Management and Conditioning Specialist
Taylormade Rehab, 1 Belle Vue, Fenny Bridges, Honiton, Devon EX14 3BJ | 07800 824557 | 07855 386634
© 2019 Taylormade | Performance & Rehabilitation Clinic. Injury Management & Conditioning Specialists | Website design by brightblueC
© 2019 Taylormade | Performance & Rehabilitation Clinic. Injury Management & Conditioning Specialists | Website design by brightblueC

 RSS Feed
RSS Feed
